
Author(s): Jyoti Dabas (Director, INFS), Praveen Budhrani (Faculty INFS), Zainab Cutlerywala (Faculty, INFS), Praveena Kuchipudi (Faculty INFS)
Research Report: Sleep and Related Health Data from 1,340 Wearable Device Users
Summary
Sleep is a critical component of overall health, influencing recovery, mental well-being, and physical performance. This report consolidates findings from a study of 1,340 wearable device users, providing insights into sleep duration, recovery, heart rate variability (HRV), and associated health impacts. Key findings indicate widespread sleep deprivation, gender differences in sleep duration, correlations between sleep quality and HRV, and the importance of addressing both sleep and stress for optimal health.
Key Insights
- Prevalence of Sleep Deprivation: Over 87% of users slept less than the recommended 8 hours per night, with nearly 20% sleeping fewer than 6 hours.
- Gender Differences in Sleep Duration: Female participants consistently had higher average sleep durations than males. For instance, during the week of October 1-7, women averaged 7.01 hours compared to 6.68 hours for men.
- Sleep and Recovery: Users with higher sleep duration, particularly deep sleep, show better recovery.
- Stress and Sleep Interplay: Shorter sleep durations were associated with higher reported stress levels. This relationship, though moderate, was statistically significant (p<0.05).
- Impact of Sleep on Health: Chronic sleep deprivation was linked to increased risks of cardiovascular diseases, impaired cognitive function, and diminished physical performance.
- Age and Sleep Trends: Average sleep duration decreased with age, particularly in users over 50, correlating with increased risks of chronic diseases.
Introduction
Sleep occupies approximately one-third of human life, yet many individuals fail to meet the recommended 7-9 hours of quality sleep per night. Wearable devices now provide extensive data to evaluate sleep patterns and their health impacts. This report explores the dimensions of sleep and its interplay with recovery, HRV, and stress among 1,340 users over four weeks.
Sleep deprivation significantly impacts cognitive and emotional health. Individuals suffering from insomnia face dramatically higher risks of anxiety and depression, with a 9.8-fold and 19.7-fold increase, respectively [1]. Physically, chronic sleep loss elevates inflammatory markers such as CRP and IL-6, contributing to heightened risks of cardiovascular diseases and metabolic disorders [2]. It also reduces testosterone levels, which are vital for muscle growth and recovery [3,4], and negatively affects heart rate variability (HRV), a crucial predictor of cardiovascular health.
Behaviorally, insufficient sleep is strongly linked to higher rates of motor vehicle accidents and workplace errors. It impairs alertness, memory, judgment, and decision-making [5]. Furthermore, chronic sleep deprivation exacerbates fatigue, limits exercise performance, and increases the likelihood of obesity, diabetes, and overall mortality. These findings highlight the urgent need to address sleep health as a cornerstone of overall well-being.
Sleep Duration and Demographics
A majority of participants (87.39%) reported sleeping less than 8 hours nightly, with age-related trends revealing that older adults (50+) slept significantly less, averaging 6.2 hours, compared to younger age groups who averaged 6.9 hours.
More worryingly, 18.2% of users slept less than 6 hours on average, where men comprise 19.5% of those sleeping less than 6hours and only 14.7% women from the sample slept for less than 6 hours.
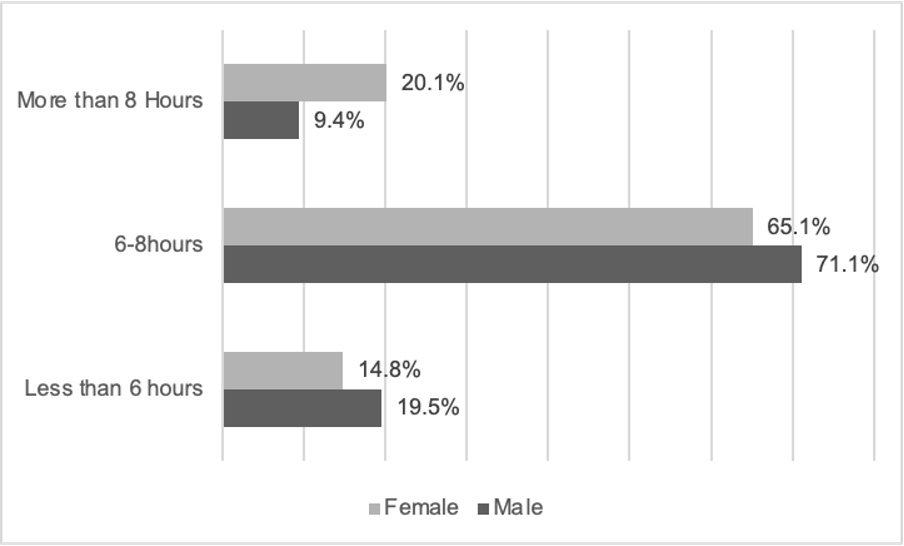 Figure 1: Sleep Duration Stratification of Sampled Population by Gender (FITTR-INFS Sleep Study, 2025)
Figure 1: Sleep Duration Stratification of Sampled Population by Gender (FITTR-INFS Sleep Study, 2025)
A systematic review shows evidence that a duration of 7-8 hours of sleep is favourably associated with overall health in both adult and older populations [6]. Further that age increases, short sleep duration is associated with a risk of developing chronic disease and high multimorbidity (p<0.001) [7,8].
While gender-specific trends highlighted that females consistently had higher average sleep durations than males. For instance, females averaged 7.01 hours compared to 6.68 hours for males. These findings align with previous research indicating that women generally report longer sleep durations than men. For instance, a study on older Indian adults found significant gender differences in sleep quality and duration, with women experiencing longer sleep durations [9]. Another study highlights the importance of considering gender differences in sleep health interventions and the potential benefits of using wearable technology for accurate sleep monitoring [10].
Recovery and Stress
Sleep is critical in recovery, influencing muscle repair, hormone regulation, and cognitive function. The restoration and rebuilding of muscles primarily occur during deep sleep stages (slow-wave sleep), where growth hormone secretion is at its peak [11]. Moreover, adequate sleep helps regulate metabolic functions, supports immune function, and improves overall cognitive functions [12]. Poor sleep, on the other hand, leads to reduced physical performance, increased fatigue, and impaired cognitive function [13]. Sleep deprivation has also been linked to heightened stress, which can have detrimental effects on both mental and physical health [14].
The observational study revealed a moderate correlation of 0.3 between recovery and overall sleep and a stronger correlation of 0.5 between recovery and deep sleep. This means that the more time spent in deep sleep (the really restful stage of sleep when the body repairs itself), the better the recovery is likely to be. Deep sleep seems to play a bigger role in helping the body recharge compared to just sleeping longer in general.
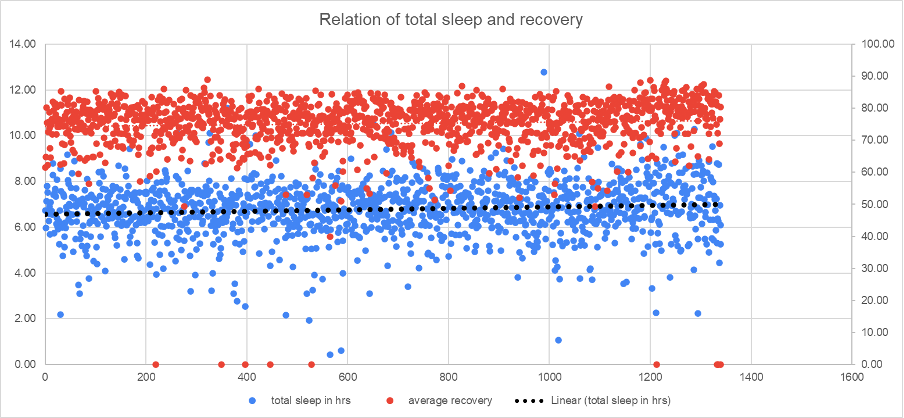 Figure 2: Positive and relatively weaker correlation between Recovery and Total Sleep (N=1340; r=0.32) (FITTR-INFS Sleep Study, 2025)
Figure 2: Positive and relatively weaker correlation between Recovery and Total Sleep (N=1340; r=0.32) (FITTR-INFS Sleep Study, 2025)
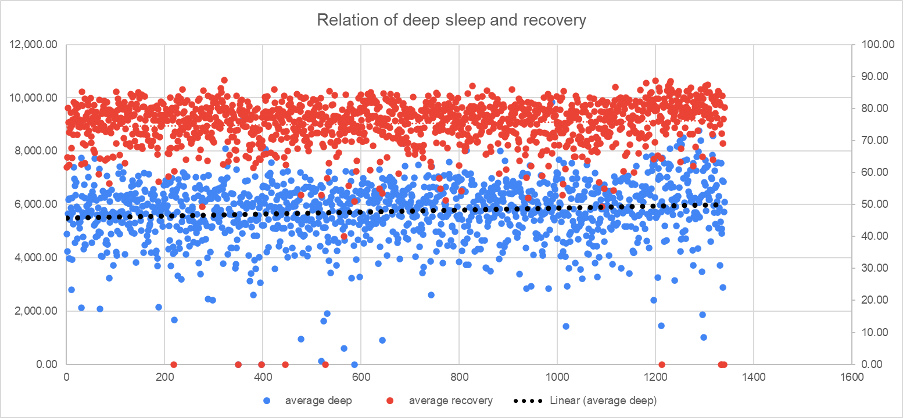 Figure 3: Positive and stronger correlation between Recovery and Deep Sleep (N=1340; r=0.46) (FITTR-INFS Sleep Study, 2025)
Figure 3: Positive and stronger correlation between Recovery and Deep Sleep (N=1340; r=0.46) (FITTR-INFS Sleep Study, 2025)
Heart rate variability (HRV) serves as a key marker of recovery. High HRV indicates robust autonomic balance and recovery [15], while low HRV reflects stress or overtraining [16]. With respect to gender nuances, the data revealed differences in sleep and recovery metrics. While females slept slightly longer on average, they reported higher resting heart rate (RHR), potentially reflecting differences in physiological and autonomous recovery mechanisms.
Interestingly, males showed marginally better heart rate variability (HRV), suggesting a mediating variable like physical activity or perceived stress to be of significance despite shorter sleep durations. However, these findings must be interpreted cautiously due to the variability inherent in averages and the limitations of the sample size, which may not fully represent broader populations.
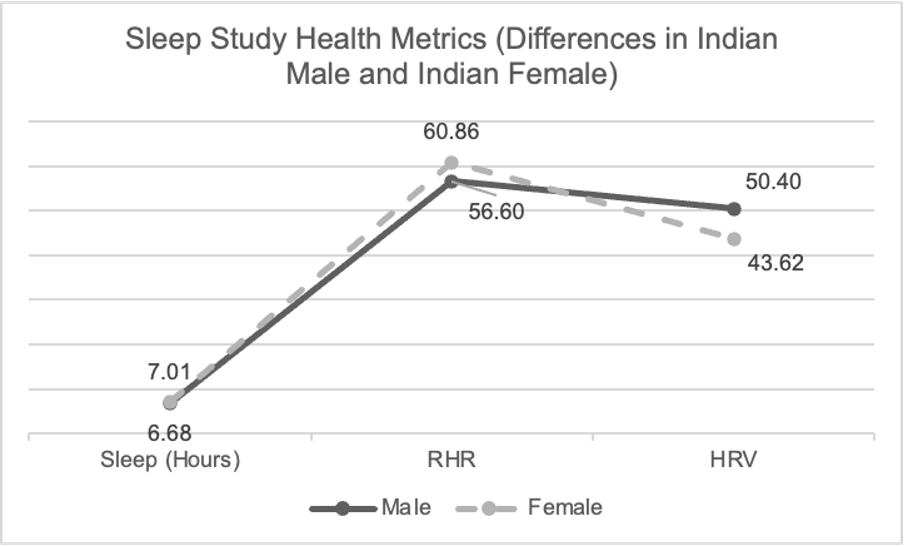 Figure 4: Gender differences in Health Metrics (FITTR-INFS Sleep Study, 2025)
Figure 4: Gender differences in Health Metrics (FITTR-INFS Sleep Study, 2025)
Overall, shorter sleep durations were associated with higher stress levels. Though the correlation was moderate, it was statistically significant (p<0.05). These findings align with prior research indicating that insufficient sleep exacerbates stress, creating a negative feedback loop that further diminishes sleep quality [17,18].
Health Implications of Poor Sleep
Sleep deprivation profoundly affects cognitive, emotional, and physical health. Studies indicate that individuals sleeping fewer than 7 hours per night face a 1.7-fold increase in injury risk and elevated levels of inflammatory markers like CRP and IL-6. Additionally, sleep deprivation correlates with reduced testosterone levels, impaired muscle growth, and heightened cardiovascular risks.
Role of Wearable Devices in Sleep Monitoring
The HART wearable device provided granular insights into users’ sleep patterns, recovery metrics, and HRV. Regular monitoring through such devices enables early detection of sleep deficiencies and helps users adopt corrective measures, ultimately improving health outcomes. Research has shown that wearable technology also enhances therapy engagement, particularly for patients undergoing treatment for sleep disorders [19].
Conclusion
The data from 1,340 wearable device users underscores the importance of adequate sleep for physical and mental health. Chronic sleep deprivation is pervasive, particularly among males and older adults, and is associated with significant health risks. HRV emerges as a valuable biomarker for recovery, closely linked to sleep quality. Gender-specific trends and the interplay between sleep and stress further highlight the need for tailored interventions. Leveraging wearable devices to monitor sleep and recovery offers a pathway to mitigate health risks and enhance well-being.
Recommendations
- Promote Sleep Education: Raise awareness about the health implications of sleep deprivation and the benefits of quality sleep.
- Utilize Wearable Technology: Encourage the use of devices to track sleep and HRV, providing actionable feedback for individuals.
- Targeted Interventions for High-Risk Groups: Implement sleep improvement programs for older adults, males, and individuals with chronic sleep deprivation.
- Address Sleep-Stress Interaction: Develop holistic approaches that simultaneously target stress reduction and sleep improvement.
- Incorporate Sleep Metrics in Health Assessments: Include sleep and HRV data in routine health check-ups to identify and address potential risks early.
Acknowledgements
The authors would like to acknowledge the support from FITTR (Squats Fitness Pvt Ltd) in providing user anonymised data for this study. Further, the support in understanding how the metrics were calculated or read from the wearable device (HART Ring), was instrumental in deriving relevant conclusions. Sincere thanks to Jitendra Chouksey for the insights, review and guidance.
References
- Oh, Chang-Myung et al. “The Effect of Anxiety and Depression on Sleep Quality of Individuals With High Risk for Insomnia: A Population-Based Study.” Frontiers in neurology vol. 10 849. 13 Aug. 2019, doi:10.3389/fneur.2019.00849
- Mullington, J.M., et al., Sleep loss and inflammation. Best Pract Res Clin Endocrinol Metab, 2010. 24(5): p. 775-84.
- Leproult, R. and E. Van Cauter, Effect of 1 week of sleep restriction on testosterone levels in young healthy men. Jama, 2011. 305(21): p. 2173-4.
- Craven, J., et al., Effects of Acute Sleep Loss on Physical Performance: A Systematic and Meta- Analytical Review. Sports Med, 2022. 52(11): p. 2669-2690.
- Killgore, W.D.S., Effects of sleep deprivation on cognition, in Progress in Brain Research, G.A. Kerkhof and H.P.A.v. Dongen, Editors. 2010, Elsevier. p. 105-129.
- Chaput, J. P., Dutil, C., Featherstone, R., Ross, R., Giangregorio, L., Saunders, T. J., Janssen, I., Poitras, V. J., Kho, M. E., Ross-White, A., & Carrier, J. (2020). Sleep duration and health in adults: an overview of systematic reviews. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme, 45(10 (Suppl. 2)), S218–S231. https://doi.org/10.1139/apnm-2020-0034
- Åkerstedt, T., Ghilotti, F., Grotta, A., Bellavia, A., Lagerros, Y. T., & Bellocco, R. (2017). Sleep duration, mortality and the influence of age. European journal of epidemiology, 32(10), 881–891. https://doi.org/10.1007/s10654-017-0297-0
- Sabia, S., Dugravot, A., Léger, D., Ben Hassen, C., Kivimaki, M., & Singh-Manoux, A. (2022). Association of sleep duration at age 50, 60, and 70 years with risk of multimorbidity in the UK: 25-year follow-up of the Whitehall II cohort study. PLoS medicine, 19(10), e1004109. https://doi.org/10.1371/journal.pmed.1004109
- de Zambotti, M. et al. (2024) ‘State of the science and recommendations for using wearable technology in sleep and circadian research’, Sleep, 47(4). Available at: https://doi.org/10.1093/SLEEP/ZSAD325.
- Jaiswal, S.J. et al. (2024) ‘Using New Technologies and Wearables for Characterizing Sleep in Population-based Studies’, Current Sleep Medicine Reports, 10(1), pp. 82–92. Available at: https://doi.org/10.1007/S40675-023-00272-7/TABLES/1.
- Van Cauter, E., Leproult, R., & Plat, L. (2000). Age-related changes in slow wave sleep and REM sleep and relation with growth hormone and cortisol levels in healthy men. JAMA, 284(7), 861-868.
- Walker, M. (2017). Why We Sleep: Unlocking the Power of Sleep and Dreams. Scribner.
- Chtourou, H., & Souissi, N. (2012). The effect of sleep deprivation on sport performance: A meta-analysis. Sleep Medicine Reviews, 16(1), 17-28.
- Hirshkowitz, M., Whiton, K., Albert, S. M., et al. (2015). National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health, 1(1), 40-43.
- Shaffer, F., & Ginsberg, J. P. (2017). An overview of heart rate variability metrics and norms. Frontiers in Public Health, 5, 258.
- Plews, D. J., Laursen, P. B., Kilding, A. E., & Buchheit, M. (2012). heart rate variability and training intensity in elite endurance athletes. European Journal of Applied Physiology, 112(1), 361-371.
- Blaxton, J.M. et al. (2017) ‘Relationships Among Nightly Sleep Quality, Daily Stress, and Daily Affect’, The Journals of Gerontology: Series B, 72(3), pp. 363–372. Available at: https://doi.org/10.1093/GERONB/GBV060.
- Zhang, J. et al. (2024) ‘Effects of stress on sleep quality: multiple mediating effects of rumination and social anxiety’, Psicologia: Reflexao e Critica, 37(1), pp. 1–10. Available at: https://doi.org/10.1186/S41155-024-00294-2/TABLES/6.
- Huang, W. et al. (2024) ‘Association of perceived stress and sleep quality among medical students: the mediating role of anxiety and depression symptoms during COVID-19’, Frontiers in Psychiatry, 15, p. 1272486. Available at: https://doi.org/10.3389/FPSYT.2024.1272486/BIBTEX.